Physician Resources
The first topic we’d like to discuss is what we consider to be the pillars or key elements in developing a high-quality, high-value AF program.
This realization came in 2013. At that juncture, I made a strategic decision that was career-altering for me, which was to treat all my patients as though they were participants in a clinical trial.
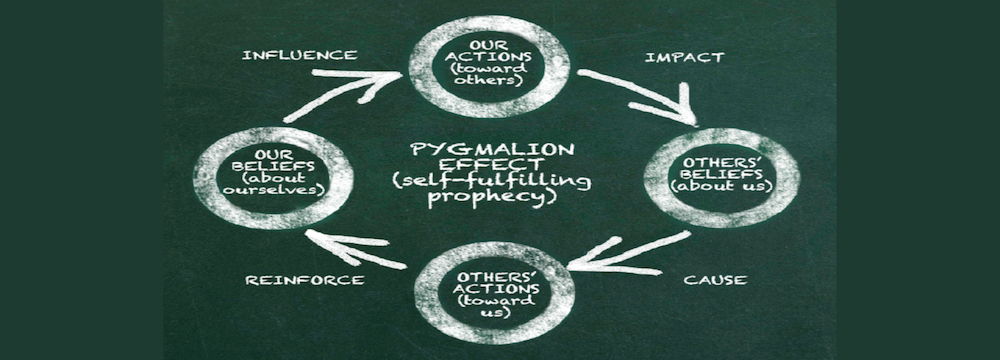
There is compelling data demonstrating that patients fare better when enrolled in a clinical trial, even if they’re assigned to a placebo group, compared to the general population. Other studies have indicated that this improvement is not solely attributable to the clinical trial itself but rather due to the standardization of care and the establishment of a process that guides patients through their journey, starting from diagnosis, initial treatment, ablation, and follow-up. Implementing a standardized approach results in better patient care.
It’s been 10 years since I started implementing the strategies we considered to be the pillars or key elements in developing a high-quality, high-value AF program:
1. Standardize Care
Similar to clinical trials, it’s crucial to determine when you’ll see your patients, the time intervals, the required tests for a comprehensive assessment, and, if you opt for ablation, how the procedure will be conducted, as well as the timing for follow-up appointments.
Standardizing care is a highly effective means of reducing costs and eliminating variations. For most patients, you can place them on a well-defined path. Once you’ve standardized care, especially if you’re focused on conducting a higher number of AF ablations, it becomes imperative to collect outcomes.
2. Collection of Outcome Data
Collecting outcomes data for all your procedures is essential. In the case of elective invasive procedures with associated risks, it’s crucial to be aware of complication rates, one-year post-ablation outcomes, and the overall well-being and improved condition of your patients.
3. Enhancing EP Lab Quality and Efficiency
Only after standardizing care, gathering outcomes data, and gaining an understanding of the operations within your EP lab and your patient population should you shift your attention towards improving efficiency.
This article is an invitation for you to map out your entire patient journey. Consider these questions:
- From the moment a patient is referred to you, what is the referral process like leading up to the clinic evaluation?
- If there is a decision to go on with a procedure, how is the consent process managed?
- How are shared decision-making discussions documented?
- What is the process for scheduling the patient?
It’s essential to map each step, as this is the only way to identify bottlenecks effectively.
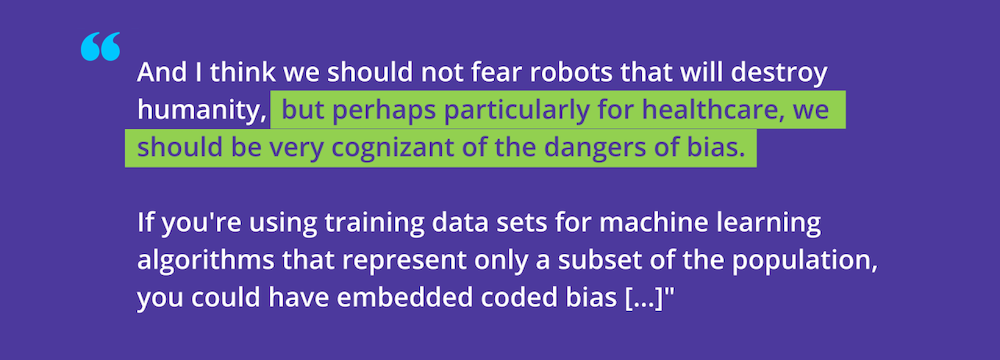
Over a decade ago, as we initiated our respective journeys in outcomes data collection and quality improvement within our institutions, we took what might be considered a disruptive approach by involving physicians outside the confines of our institution in outcomes data collection. We have now transformed outcomes data collection and quality improvement into a collaborative effort, involving dozens of institutions and over 100 electrophysiologists. We employ similar approaches to outcomes data collection, allowing us to collectively share data, learn from each other, and drive improvements in quality.
Our aim was not merely to gain insight into the practices at our individual institutions. Instead, we aspired to make this a widely applicable concept and process, ensuring its reproducibility across multiple institutions, with the hope of it becoming a standard practice.
Ultimately, what we envision building is a learning health system.