Afib Medications
Atrial fibrillation and the newer blood thinners – Pradaxa, Xarelto, and Eliquis
If you have afib, you should learn about 3 different medication classes that may be used in your therapy:
- Rhythm Control medications or anti-arrhythmic drugs
- Rate Control medications
- Oral Anticoagulants or blood thinners
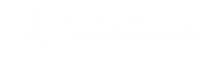
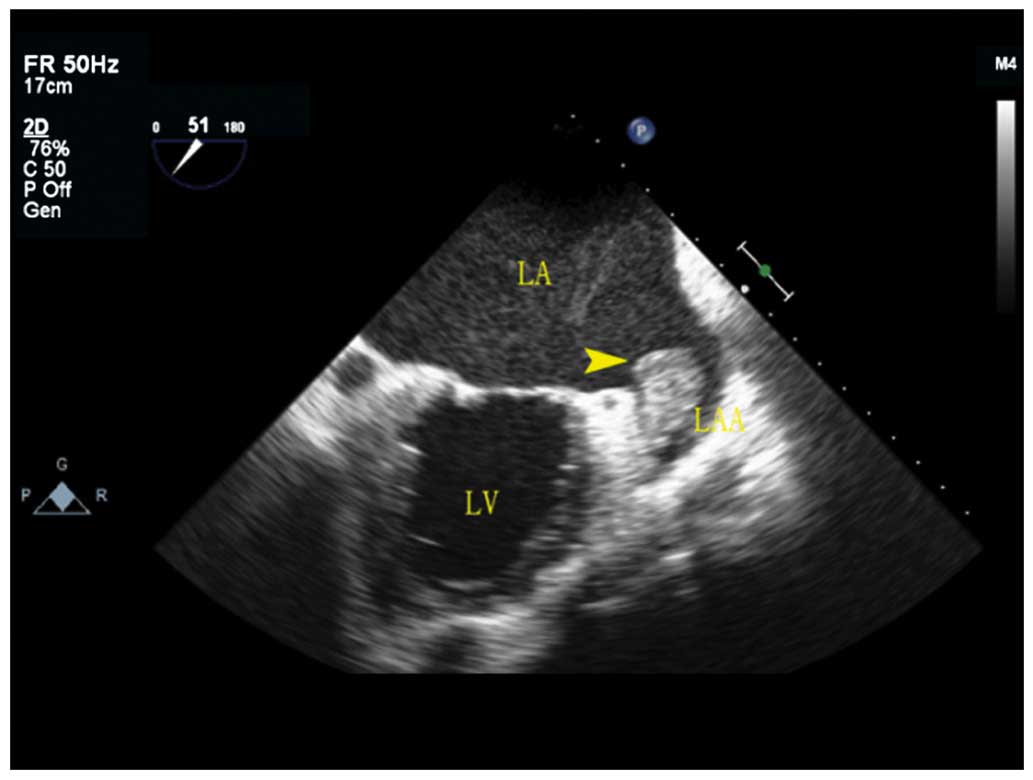
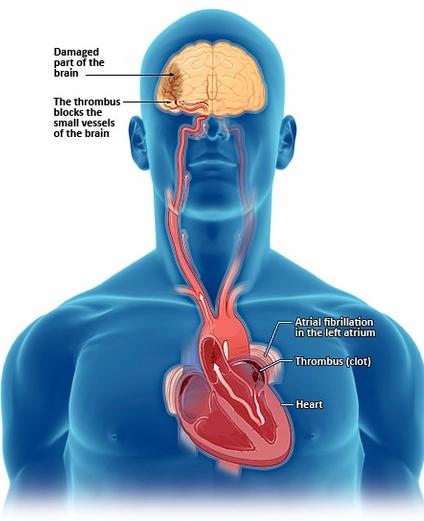
Atrial fibrillation is the most common heart rhythm disorder and it is associated with an increased risk of strokes. Strokes occur when blood clots are formed in the left atrium and if they dislodge they may cut off blood supply to a part of the brain.
Anticoagulants work by preventing the formation of blood clots. Warfarin, Pradaxa, Xarelto, and Eliquis are the blood thinners available in the US.
What are blood thinners and why are they used?
Blood thinners are used to prevent strokes in patients who have atrial fibrillation and are at risk. They make your blood less likely to clot. In patients with Afib, they are used to prevent the formation of blood clots in the left atrium – which are the cause of strokes.
Warfarin
Up until a few years ago, the only option available was warfarin.
Warfarin is a drug proven to reduce strokes. In patients with atrial fibrillation, warfarin can decrease the risk of strokes by 60-70%. However, this benefit comes at a price. It is at the expense of an increased risk of intracranial bleeding, other bleeding and a significant change in a patient’s lifestyle. Patients taking warfarin should have a limited and steady intake of foods containing vitamin K (green leafy vegetables). Furthermore, there is a need for frequent blood checks to see if the blood is adequately anticoagulated. It also has many drug-drug interactions.
Therefore, although warfarin has proven benefits, it is a very cumbersome drug. It has side effects and many interactions with food and other drugs, and it requires constant monitoring.
The Novel Anticoagulants – Dabigatran, Rivaroxaban and Apixaban
Recently, newer blood thinners have become available. The so called “novel anticoagulant agents” approved in the United States are:
-
Dabigatran (Pradaxa)
-
Rivaroxaban (Xarelto)
-
Apixaban (Eliquis)
All three drugs were approved after large clinical trials, including tens of thousands of patients, were conducted. The trials were designed to show that the each one of these drugs was at least non-inferior to Coumadin and they have all managed to do that. Further analysis and clinical practice has shown however that they are probably superior to Coumadin.
The new drugs have all produced a significantly lower risk of hemorrhagic strokes. Hemorrhagic strokes are caused by blood thinners; they are essentially the price we pay for using these agents to decrease strokes.
The novel anticoagulants have many similarities:
- Mode of action
- No need for frequent blood work to see if the levels are in the right range
- No interaction with food
- Very few drug interactions
- Very tolerable – number of patients stopping the meds because of side effects is similar to coumadin
Signs and Symptoms of bleeding while on a blood thinner
The newer blood thinners are designed to make your blood less likely to clot. Therefore, it is to be expected that there is an increased risk of bleeding. If you are started on one of the novel anticoagulants, please contact your doctor or seek medical care if you have any signs or symptoms of bleeding:
- any unexpected, severe, or uncontrollable bleeding
- unusual or unexpected bruising
- coughing up or vomiting blood; or vomit that looks like coffee grounds
- pink or brown urine; red or black stools (looks like tar)
- unexpected pain, swelling, or joint pain
- headaches and feeling dizzy or weak
What is your risk of bleeding?
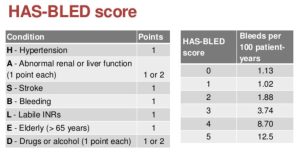
The risk of bleeding with the newer blood thinners and with Coumadin is increased in some patients. The HAS-BLED bleeding risk score is used to see what your risk of bleeding is. The more risk factors you have, the higher the risk.
Blood thinners and Surgery
Blood thinners may need to be stopped, if possible, before surgery or medical or dental procedures. If you are taking coumadin it may have to be stopped 5 days before your procedure. The newer anticoagulants can be stopped 1 or 2 days before your procedure, depending on you kidney function and the procedure you are having. Be sure to discuss with you doctor before stopping. Risks and benefits of stopping it for a few days need to be discussed and taken into consideration.
Afib and Newer Blood Thinners
If you have Afib and your stroke risk is elevated, oral anticoagulation (blood thinners) can be used to reduce the risk. Talk to your doctor about it!
Atrial Fibrillation (Afib) is a condition that can impact your quality of life and cause strokes. Afib treatment should be individualized to meet each patient’s needs.
Dr Jose Osorio
Miami, FL
Read More About AFib: