Comprehensive AFib Guide
This AFib Guide offers a complete journey through understanding, diagnosing, and treating atrial fibrillation. We cover everything from symptoms and risks to advanced treatment options like ablation and stroke prevention. Click the sections below to navigate specific topics.
Comprehensive AFib Guide: Diagnosis, Treatment, and Long-Term Care
Table of Contents
-
Introduction to Atrial Fibrillation (AFib)
-
Understanding the Heart’s Electrical System and Normal Heart Function
-
What is Atrial Fibrillation (AFib)?
-
Diagnosing Atrial Fibrillation (AFib)
-
Treatment Options for Atrial Fibrillation (AFib)
-
AFib Ablation – A Closer Look at AFib Ablation Procedures
-
Stroke Risk and Prevention in AFib Patients
-
Conditions That Cause or Worsen AFib: Sleep Apnea, Obesity, Hypertension, and Alcohol
-
Frequently Asked Questions about AFib
-
Conclusion and Next Steps
Section 1: Introduction to Atrial Fibrillation (AFib)
Atrial Fibrillation (AFib) is the most common type of heart rhythm disorder (arrhythmia), affecting millions of individuals worldwide. This condition primarily affects the atria, the heart’s upper chambers, causing them to beat rapidly and irregularly. AFib can significantly impact an individual’s health and quality of life, increasing the risk of complications like stroke, heart failure, and, in severe cases, reduced life expectancy.
AFib often begins subtly, with brief episodes that may be barely noticeable. As the condition progresses, episodes may become more frequent and longer-lasting, potentially leading to a permanent form of AFib. While AFib is usually not immediately life-threatening, it’s crucial to diagnose and treat it early to manage symptoms and prevent severe complications.
Key Facts About AFib
- Prevalence: Over 33 million people globally are diagnosed with AFib, and its prevalence increases with age, making it a common condition in older adults.
- Risk of Complications: Patients with AFib are five times more likely to have a stroke, as blood can pool in the atria, leading to clot formation.
- Lifestyle Impact: AFib can affect physical activities, social interactions, and overall quality of life. Fatigue, shortness of breath, and a rapid or irregular heartbeat can make even simple daily activities challenging.
For more on how AFib develops and impacts heart function, read What is Atrial Fibrillation?
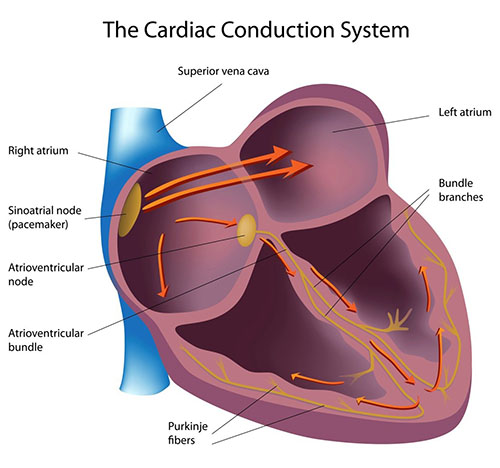
Understanding the Mechanics of AFib
In a healthy heart, electrical impulses flow in a regular, organized pattern from the sinoatrial (SA) node, the heart’s natural pacemaker. This impulse travels through the atria to the atrioventricular (AV) node and into the ventricles, producing a coordinated heartbeat. However, in AFib, the electrical signals in the atria become chaotic, leading to rapid and irregular contractions that disrupt the heart’s regular pumping function.
This abnormal rhythm, called fibrillation, causes the atria to quiver rather than contract fully, preventing efficient blood flow. The irregularity in blood flow can lead to clot formation, particularly in a small, pouch-like area of the heart called the left atrial appendage. If a clot dislodges and travels to the brain, it can block an artery and cause a stroke.
What Causes AFib?
AFib can result from several underlying conditions and lifestyle factors:
- Cardiovascular Conditions: Hypertension, coronary artery disease, and heart failure are common precursors.
- Age and Genetics: Advanced age and family history increase the likelihood of developing AFib.
- Sleep Apnea: Obstructive sleep apnea is highly correlated with AFib due to its impact on heart function.
- Lifestyle Factors: Obesity, alcohol consumption, smoking, and high-stress levels have all been linked to AFib.
Each of these factors influences the heart’s structure and electrical signaling, making AFib more likely.
Importance of Early Diagnosis and Treatment
Since AFib is a progressive condition, early diagnosis is crucial. Treating AFib early can slow its progression and help manage symptoms effectively. Left untreated, AFib can lead to more severe health issues, including:
- Stroke: AFib increases the risk of ischemic stroke by promoting clot formation.
- Heart Failure: The irregular heart rhythm can weaken the heart over time, leading to heart failure.
- Decreased Quality of Life: Symptoms like fatigue, dizziness, and palpitations often disrupt daily activities and can lead to emotional distress.
Through lifestyle changes, medication, and medical procedures, AFib can be managed effectively, allowing patients to maintain a high quality of life. For a deeper understanding of AFib symptoms and treatment, visit AFib Treatment Options.
Goals of AFib Treatment and Management
Managing AFib involves a comprehensive approach that addresses both symptoms and underlying causes. Treatment goals often include:
- Preventing Blood Clots and Reducing Stroke Risk: Using anticoagulant medications or procedures like the Watchman device to reduce clot formation.
- Controlling Heart Rate and Rhythm: Medications or ablation procedures can help maintain a normal rhythm.
- Improving Quality of Life: Minimizing symptoms so patients can engage in regular activities without disruption.
For most patients, an individualized treatment plan can make a significant difference in managing AFib and preventing progression. The AFib Clinic in Miami, led by Dr. Jose Osorio, specializes in creating personalized management plans for each patient based on their unique health profile.
Section 2: Understanding the Heart’s Electrical System and Normal Heart Function
To comprehend atrial fibrillation (AFib), it’s essential first to understand how the heart’s electrical system works under normal circumstances. The heart operates through a well-coordinated system that regulates each heartbeat, enabling effective blood flow throughout the body. In this section, we will explore the heart’s structure, its electrical conduction system, and how disruptions in these mechanisms lead to arrhythmias such as AFib.
For a detailed visual explanation, visit Normal Heart Rhythm.
The Heart’s Structure: Chambers and Valves
The human heart has four chambers:
- Two Upper Chambers (Atria): The right atrium receives deoxygenated blood from the body and sends it to the right ventricle. The left atrium receives oxygenated blood from the lungs and sends it to the left ventricle.
- Two Lower Chambers (Ventricles): The ventricles are responsible for pumping blood out of the heart. The right ventricle sends deoxygenated blood to the lungs, while the left ventricle pumps oxygenated blood throughout the body.
Each chamber is separated by valves that ensure blood flows in a single direction. The heart’s powerful and rhythmic contractions are primarily managed by the ventricles, especially the left ventricle, which is crucial for maintaining blood circulation.
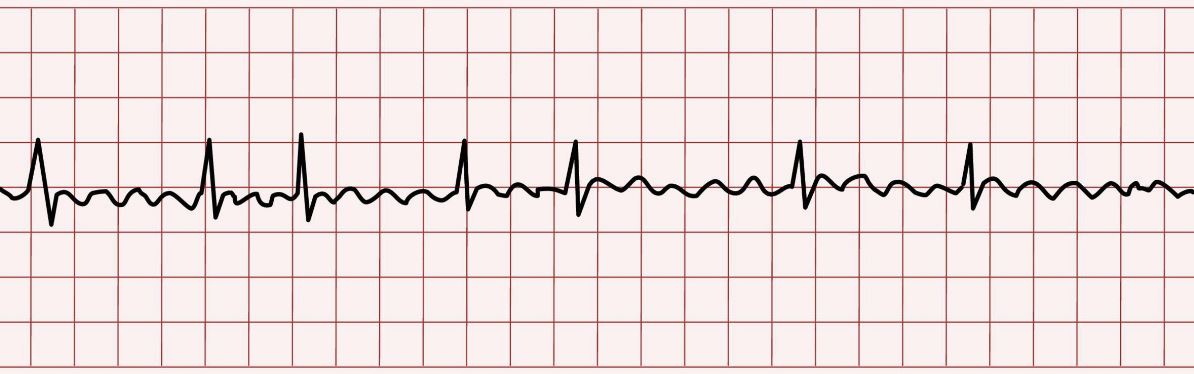
The Heart’s Electrical Conduction System
The heart’s rhythm is controlled by its electrical conduction system, a network of cells and pathways that carry electrical impulses, ensuring synchronized heartbeats. The primary components of this system include:
- The Sinoatrial (SA) Node: Known as the heart’s natural pacemaker, the SA node generates electrical impulses that set the heart’s rhythm. Located in the right atrium, the SA node initiates each heartbeat, controlling the heart rate and adjusting it as needed—such as during physical activity or rest.
- The Atrioventricular (AV) Node: Situated between the atria and ventricles, the AV node receives the electrical impulse from the SA node. It introduces a slight delay, allowing the ventricles time to fill with blood before contracting. This delay is crucial for maintaining efficient blood flow from the atria to the ventricles.
- The His-Purkinje Network: After passing through the AV node, the electrical impulse travels through the His-Purkinje network—a series of specialized fibers that distribute the impulse to the right and left ventricles, prompting them to contract in unison. This synchronized contraction pumps blood out of the heart and throughout the body.
A coordinated sequence of electrical impulses ensures the heart pumps efficiently. The process works as follows:
- Impulse Generation: The SA node generates an electrical impulse that spreads across the atria, causing them to contract and push blood into the ventricles.
- AV Node Delay: The impulse reaches the AV node, where a brief delay allows the ventricles to fill with blood.
- Ventricular Contraction: The impulse then travels through the His-Purkinje fibers, triggering the ventricles to contract and send blood to the lungs and body.
When this electrical sequence is maintained, the heart operates in a regular, rhythmic manner known as sinus rhythm.
Disruptions in the Electrical System: How Arrhythmias Occur
In a healthy heart, the SA node, AV node, and His-Purkinje network work seamlessly to produce a steady heartbeat. However, when this electrical flow is disrupted, the heart may beat irregularly or too quickly. These disruptions are referred to as arrhythmias. Atrial fibrillation, the most common type of arrhythmia, results from erratic electrical signals in the atria, causing them to quiver or fibrillate rather than contract regularly.
In AFib, several changes occur in the heart’s electrical system:
- Erratic Signals in the Atria: Instead of one organized signal from the SA node, multiple rapid and chaotic signals are generated in the atria, especially near the pulmonary veins.
- Irregular Ventricular Response: These erratic signals bombard the AV node, which transmits some of them to the ventricles, resulting in an irregular and often rapid heartbeat.
Why AFib Disrupts Heart Function
AFib affects the heart’s ability to pump blood effectively. Since the atria no longer contract in a coordinated way, they contribute less to the heart’s overall pumping function. Blood can pool in the atria, particularly in the left atrial appendage, which significantly raises the risk of blood clot formation. If a clot escapes and travels to the brain, it can cause a stroke. Therefore, understanding and managing AFib is essential to minimizing risks associated with blood flow irregularities and potential clot formation.
For more on AFib-related stroke risks, refer to AFib & Stroke Risk.
Key Takeaways: Heart Function and AFib
- Normal Heartbeat: A normal, sinus rhythm relies on a precise sequence of electrical impulses from the SA node through the AV node to the ventricles.
- AFib Disruption: AFib interrupts this rhythm, creating chaotic electrical signals that prevent the atria from contributing effectively to blood flow.
- Stroke Risk: The risk of clot formation in the left atrial appendage underscores the need for stroke prevention in AFib management.
Understanding how the heart’s electrical system functions under normal and AFib conditions offers valuable insight into why AFib requires careful management and tailored treatment strategies. With this foundation, patients can better understand their condition, make informed decisions about treatment options, and take steps to improve their quality of life.
For further insights on how AFib affects heart function, check out our page on Normal Heart Rhythm.
Section 3: What is Atrial Fibrillation (AFib)?
Atrial fibrillation, commonly referred to as AFib, is the most prevalent type of arrhythmia—a condition in which the heart’s normal rhythm is disrupted. In AFib, the atria (the upper chambers of the heart) experience erratic electrical impulses, leading to rapid and irregular heartbeats. This section explores AFib in depth, including its causes, symptoms, types, and potential complications. By understanding the mechanics of AFib and its impact on overall health, patients can make more informed decisions about their care and treatment options.
For a more detailed description, please refer to What is Atrial Fibrillation (AFib)?.
What Happens in Atrial Fibrillation?
In a normal heart, the sinoatrial (SA) node generates regular electrical impulses that follow a predictable path, resulting in a steady heartbeat. However, in AFib, multiple rapid, chaotic signals are generated, especially near the pulmonary veins, causing the atria to quiver instead of contracting in a coordinated manner. This “fibrillation” of the atria means blood is not pumped efficiently into the ventricles. As a result, the ventricles also beat irregularly, which can lead to a rapid, erratic heartbeat.
This irregularity disrupts the heart’s ability to pump blood effectively and may lead to symptoms such as heart palpitations, fatigue, and shortness of breath.
Common Causes and Risk Factors for AFib
While AFib can develop without any apparent reason, several common risk factors increase the likelihood of experiencing the condition. These include:
- Age: AFib is more common in individuals over 60, and the risk continues to increase with age.
- Obesity: Increased body mass can enlarge the heart and put more strain on it, raising AFib risk.
- Obstructive Sleep Apnea (OSA): OSA affects breathing during sleep, leading to increased atrial stretch and a higher risk of AFib. Treating OSA with CPAP or weight loss can help.
- Hypertension (High Blood Pressure): Uncontrolled high blood pressure causes structural changes in the heart, which may lead to AFib.
- Heart Disease: Conditions like coronary artery disease, heart failure, and previous heart attacks can predispose individuals to AFib.
- Other Medical Conditions: Diabetes, thyroid disorders, and chronic lung diseases are also associated with a higher AFib risk.
- Lifestyle Factors: Excessive alcohol and stimulant use, as well as high stress levels, can increase the likelihood of AFib episodes.
For a deeper dive into these causes and risk factors, please visit AFib Overview.
Symptoms of Atrial Fibrillation
AFib symptoms vary significantly among patients. Some experience intense discomfort, while others may have no noticeable symptoms. Common AFib symptoms include:
- Heart Palpitations: Sensation of a racing, fluttering, or irregular heartbeat.
- Fatigue: Decreased energy levels, especially during physical activities.
- Dizziness or Lightheadedness: Feeling faint or unsteady.
- Shortness of Breath: Difficulty breathing or breathlessness, even during mild activities.
- Chest Discomfort: Mild to moderate chest pain or pressure.
- Exercise Intolerance: Increased fatigue or discomfort during physical exertion.
Patients who experience these symptoms are encouraged to seek evaluation, as AFib is associated with serious complications, particularly stroke.
For further information on symptoms, check our Symptoms of AFib page.
Types of Atrial Fibrillation
Understanding the different types of AFib is crucial for determining the appropriate treatment approach. AFib is classified into four primary types based on its frequency and persistence:
- Paroxysmal AFib: Episodes occur sporadically, typically lasting less than 24 hours, and resolve on their own. This type is often seen earlier in the disease process, especially in patients with fewer risk factors.
- Persistent AFib: Episodes that continue for more than seven days and do not resolve on their own. Medical intervention, such as medication or a procedure, is usually required to restore normal rhythm.
- Longstanding Persistent AFib: Continuous AFib lasting longer than a year, often requiring a more complex treatment approach, with reduced chances of reestablishing a normal rhythm.
- Permanent AFib: In cases where attempts to restore normal rhythm are unsuccessful or impractical, AFib is accepted as a permanent condition. Treatment focuses on managing symptoms and preventing complications.
Recognizing these types underscores the importance of early diagnosis and intervention, as AFib tends to progress over time, potentially becoming more challenging to manage. For more details, visit Types of AFib.
Complications Associated with AFib
AFib is associated with several potentially life-threatening complications, particularly:
- Increased Stroke Risk: Blood pooling in the left atrial appendage during AFib increases the likelihood of clot formation, which, if dislodged, can cause a stroke. Patients with AFib are five times more likely to experience a stroke than those without the condition.
- Heart Failure: The irregular and rapid heart rate associated with AFib can weaken the heart, potentially leading to heart failure. Over time, prolonged AFib can impair the heart’s ability to pump effectively, resulting in symptoms such as swelling, fatigue, and shortness of breath.
- Decline in Quality of Life: Frequent AFib episodes can significantly impact daily life, limiting physical activity and affecting mental well-being. Chronic fatigue, anxiety, and reduced exercise tolerance are common issues for AFib patients.
- Dementia and Cognitive Decline: Studies have shown a link between AFib and an increased risk of cognitive decline and dementia, particularly in patients who experience prolonged episodes. This may be due to reduced blood flow to the brain or frequent small clots.
Understanding these potential complications reinforces the importance of AFib management, including preventive measures and lifestyle modifications.
For more information on AFib and its complications, visit our AFib & Stroke Risk page.
Key Takeaways: What is Atrial Fibrillation?
- AFib is the most common arrhythmia, affecting the heart’s ability to pump blood effectively.
- Risk Factors: Include age, obesity, hypertension, sleep apnea, and lifestyle factors.
- Symptoms: AFib symptoms range from palpitations to fatigue, chest discomfort, and shortness of breath.
- Types of AFib: Paroxysmal, persistent, longstanding persistent, and permanent.
- Complications: Stroke, heart failure, and quality of life decline are the most significant risks associated with untreated AFib.
This comprehensive understanding of AFib’s causes, symptoms, and types prepares patients for the following sections, which will explore AFib diagnosis and treatment options.
Section 4: Diagnosing Atrial Fibrillation (AFib)
Atrial fibrillation diagnosis is a critical step toward understanding and managing the condition effectively. Due to the episodic nature of AFib, diagnosis can sometimes be challenging, especially in the early stages. This section covers the methods, tools, and procedures available to diagnose AFib accurately, from ECGs and wearable technology to advanced monitoring techniques.
Visit our AFib Diagnosis page for more information.
Importance of Timely Diagnosis
AFib often begins as paroxysmal episodes, which are intermittent and may only last a few minutes to hours. These episodes can go undetected if they are infrequent, leading to delays in diagnosis. Without timely diagnosis and intervention, AFib can progress to a more persistent form, increasing the risk of complications such as stroke and heart failure. Thus, prompt detection and monitoring are essential, allowing for early intervention and potentially more successful management of the condition.
Diagnostic Tools and Methods
1. Electrocardiogram (ECG)
- An ECG is the primary tool for diagnosing AFib. It records the heart’s electrical activity, displaying it as waves on a graph, which can reveal irregular heart rhythms.
- 12-Lead ECG: Often performed in a clinical setting, this type of ECG involves placing 10 electrodes on the patient’s body to provide a comprehensive view of the heart’s electrical activity.
- Limitations: Since AFib can be intermittent, an ECG must be performed while the patient is experiencing an episode to confirm a diagnosis.
2. Holter Monitors
- For patients with paroxysmal AFib, which comes and goes, a 24- to 48-hour Holter monitor may be recommended. This portable device records continuous heart activity, capturing AFib episodes even if the patient is asymptomatic.
- Extended Holter Monitoring: Newer devices, such as patch monitors, allow for extended monitoring (up to 14 days) without bulky equipment, enhancing patient comfort and diagnostic accuracy.
3. Implantable Loop Recorders (ILR)
- In cases where AFib episodes are infrequent but suspected, an ILR may be used. This small device, implanted under the skin, continuously records heart rhythms for up to three years, offering long-term monitoring and reliable detection of irregularities.
- Ideal for Intermittent AFib: ILRs are beneficial for detecting rare but significant arrhythmic events, particularly for patients at high stroke risk.
4. Wearable Technology

- Apple Watch and Other Smartwatches: Wearables have transformed AFib diagnosis, allowing patients to record their heart rhythm at any time. The Apple Watch, for example, uses photoplethysmography (PPG) to detect irregular pulses and offers an ECG function for a more precise reading.
- Limitations: While wearables increase early detection, especially in asymptomatic patients, they are prone to false positives, especially in younger users. A healthcare provider should confirm any readings.
- For more on how wearables assist in AFib diagnosis, refer to Apple Watch and AFib Detection.
5. Pacemakers and Defibrillators
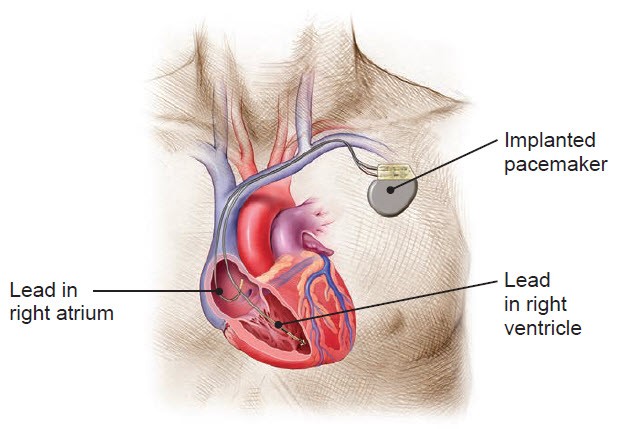
- For patients with implantable cardiac devices, such as pacemakers or defibrillators, these devices record any arrhythmic events. Physicians can review the device’s memory to assess for AFib episodes during routine checkups.
Diagnosing Paroxysmal AFib
Paroxysmal AFib, characterized by sporadic episodes, presents unique diagnostic challenges. Here’s a structured approach for detecting AFib in these cases:
- Patient Symptom Tracking: Patients are encouraged to note any palpitations, chest discomfort, dizziness, or other symptoms. Combining symptom diaries with wearable monitoring often aids in identifying patterns and potential triggers.
- Patch and Holter Monitoring: For those with infrequent but symptomatic episodes, extended Holter or patch monitors offer a non-invasive way to monitor for AFib over several days.
- Loop Recorders for Infrequent Episodes: In cases where episodes are very rare, an ILR provides continuous long-term monitoring, with automatic alerts sent to healthcare providers if AFib is detected.
Diagnosing Persistent and Permanent AFib
Persistent and permanent forms of AFib are typically easier to diagnose since the heart is consistently out of rhythm. When AFib persists for over seven days or becomes a continuous rhythm, any standard ECG can confirm the diagnosis, as the arrhythmia will be present at all times.
Diagnostic Procedures and Tests
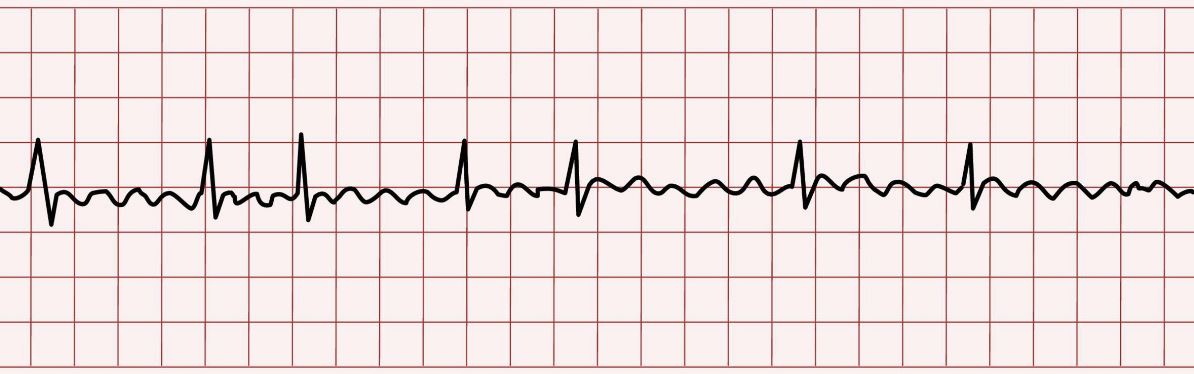
- Electrocardiogram (ECG)
- A standard ECG is the first-line test to confirm AFib, recording the heart’s rhythm during an AFib episode and providing critical information on the arrhythmia’s pattern.
- Echocardiogram
- This ultrasound-based imaging test evaluates heart structure and function, identifying potential underlying causes of AFib, such as valve disease or left atrial enlargement.
- Stress Testing
- For patients with symptoms of AFib triggered by physical exertion, stress testing helps determine how the heart responds to increased workload, revealing issues like coronary artery disease, which may exacerbate AFib.
- Blood Tests
- Blood tests assess thyroid function, electrolyte levels, and other factors that may contribute to AFib. Thyroid abnormalities, for instance, are a known trigger for AFib.
The Role of Lifestyle in AFib Diagnosis
Diagnosing AFib often involves evaluating lifestyle factors, as certain habits and conditions can contribute to AFib progression or trigger episodes. For instance, dehydration, high alcohol intake, excessive caffeine, and stress are all potential AFib triggers. Clinicians may advise lifestyle adjustments during the diagnostic process to help identify and potentially mitigate triggers.
For additional information on lifestyle’s impact on AFib, visit AFib Lifestyle and Medical Conditions.
When to See a Specialist
If AFib is suspected or confirmed, patients are generally referred to a cardiologist or electrophysiologist for further evaluation and treatment. These specialists focus on heart rhythm disorders, providing a comprehensive approach to diagnosing and managing AFib. Early referral can improve outcomes, particularly for patients who may benefit from interventional procedures like AFib ablation.
Key Takeaways: Diagnosing AFib
- Prompt diagnosis is crucial for preventing AFib progression and managing stroke risk.
- ECGs are essential for detecting AFib, but due to the condition’s episodic nature, long-term monitoring methods like Holter monitors, ILRs, and wearable technology can improve diagnostic accuracy.
- Additional tests, including echocardiograms, stress tests, and blood work, help identify underlying causes and guide treatment decisions.
- Monitoring lifestyle factors provides insights into AFib triggers, enhancing individualized treatment plans.
Section 5: Treatment Options for Atrial Fibrillation (AFib)
When managing Atrial Fibrillation (AFib), treatment focuses on three primary goals: reducing the risk of stroke, controlling symptoms to improve quality of life, and slowing the progression of AFib. AFib treatment options are diverse and range from lifestyle modifications to advanced procedures like AFib ablation. The chosen treatment plan depends on the individual’s symptoms, comorbidities, type of AFib, and overall health.
AFib treatment can be broadly categorized into medical management (medications), interventional procedures (such as ablation), and lifestyle modifications. A comprehensive treatment plan often combines these options, addressing the needs and preferences of each patient.
Goals of AFib Treatment
When treating AFib, it is essential to focus on several key goals:
- Preventing Stroke: Stroke prevention is always a primary objective. With AFib’s association with blood clots, anticoagulation (blood-thinning) therapies are often necessary to reduce the risk of clot formation.
- Controlling Heart Rate: Managing heart rate is important to reduce symptoms such as palpitations, fatigue, and dizziness. Rate control strategies aim to keep the heart rate within a target range without necessarily restoring a normal rhythm.
- Restoring and Maintaining Normal Rhythm: Rhythm control involves using medications or procedures to try to restore the heart’s normal rhythm, particularly in symptomatic patients or those who don’t respond well to rate control.
- Improving Quality of Life: Treatment should aim to minimize AFib’s impact on daily activities and overall well-being.
1. Medications for AFib Management
Medications are frequently the first line of treatment for AFib and play an essential role in both rhythm and rate control. They can help regulate heart rate, reduce the frequency of AFib episodes, and manage the risk of stroke.
a. Blood Thinners (Anticoagulants)
Anticoagulants are essential for AFib patients at risk of stroke. By preventing blood clots from forming, they reduce the risk of a clot reaching the brain and causing a stroke.
- Common Options: Warfarin (Coumadin) and Direct Oral Anticoagulants (DOACs) like apixaban (Eliquis), dabigatran (Pradaxa), rivaroxaban (Xarelto), and edoxaban (Savaysa).
- Considerations: Warfarin requires regular blood tests and dietary monitoring, while DOACs are easier to manage but may not be suitable for everyone. Anticoagulants may increase the risk of bleeding, so regular follow-up and communication with a healthcare provider are essential.

For more on blood thinners, visit our Common AFib Medications page.
b. Rate Control Medications
Rate control medications slow the heart rate without directly addressing the abnormal rhythm. By controlling the rate, these medications can help reduce AFib symptoms and allow the heart to function more effectively.
- Beta-Blockers: Medications such as metoprolol, atenolol, and bisoprolol work by reducing the heart rate, helping patients feel more comfortable during AFib episodes.
- Calcium Channel Blockers: Diltiazem and verapamil are commonly prescribed to help relax the heart muscle and reduce heart rate.
- Digoxin: Used less frequently but may be beneficial in specific cases, particularly in patients with heart failure.
c. Rhythm Control Medications (Antiarrhythmics)
For patients experiencing significant symptoms from AFib, rhythm control medications can help maintain a regular heart rhythm. These medications attempt to prevent AFib episodes or reduce their frequency.
- Common Antiarrhythmics: Flecainide, propafenone, sotalol, and amiodarone are some commonly used antiarrhythmic medications for rhythm control.
- Considerations: Antiarrhythmic drugs can have potential side effects and may not be suitable for everyone, particularly those with certain heart conditions. Regular follow-ups are essential to monitor efficacy and side effects.
To learn more about medications for AFib, visit our page on AFib Medications.
2. Cardioversion for AFib
Cardioversion is a procedure used to reset the heart to a normal rhythm. It can be achieved either electrically or chemically, depending on the patient’s condition and the physician’s recommendation.
a. Electrical Cardioversion
Electrical cardioversion involves delivering a controlled electric shock to the heart, which stops the abnormal rhythm and allows it to reset to a normal rhythm. It is typically done in a hospital setting with sedation.
- Effectiveness: This method is highly effective for restoring normal rhythm, especially in patients with paroxysmal or recent-onset persistent AFib. However, it doesn’t cure AFib, and without medications and lifestyle changes, it will most likely recur.
- Considerations: Electrical cardioversion may need to be repeated if AFib episodes recur.
b. Chemical Cardioversion
Chemical cardioversion uses intravenous or oral antiarrhythmic medications to help restore a normal heart rhythm. This option is usually employed when electrical cardioversion is not suitable or when the patient is not in immediate need of cardioversion.
- Common Medications: Amiodarone, flecainide, and propafenone may be used for chemical cardioversion.
- Considerations: The effectiveness of chemical cardioversion can vary, and it may take longer to restore normal rhythm than electrical cardioversion.
Cardioversion is often used in combination with anticoagulation therapy to reduce stroke risk before and after the procedure.
3. Catheter Ablation: A Minimally Invasive Solution for AFib
Catheter ablation is a minimally invasive procedure aimed at reducing or eliminating AFib by targeting the areas within the heart that are responsible for the abnormal electrical signals. Catheter ablation has become a common treatment for patients who do not respond to medications or prefer a more permanent solution.
Types of Catheter Ablation:
- Radiofrequency (Thermal) Ablation: Uses heat to destroy the abnormal tissue that is causing AFib.
- Cryoablation (Cold) Ablation: Uses extreme cold to freeze and destroy the targeted areas.
- Pulsed Field Ablation (PFA): A newer technology that uses electrical pulses to target AFib triggers selectively, reducing the risk of damaging surrounding structures.
Each method has its own advantages, and the choice depends on individual patient factors, physician experience, and the patient’s specific type of AFib. Ablation is performed under general anesthesia and usually requires a one-night hospital stay.
- Success Rates: Success rates for catheter ablation vary based on the type of AFib and the patient’s overall health, with paroxysmal AFib showing higher success rates. Studies show that catheter ablation has a success rate of up to 75–90% for paroxysmal AFib.
- Considerations: While effective, catheter ablation may need to be repeated if AFib returns. It is essential to follow up with a cardiologist or electrophysiologist post-procedure for optimal results.
For more on this procedure, visit our page on AFib Ablation.
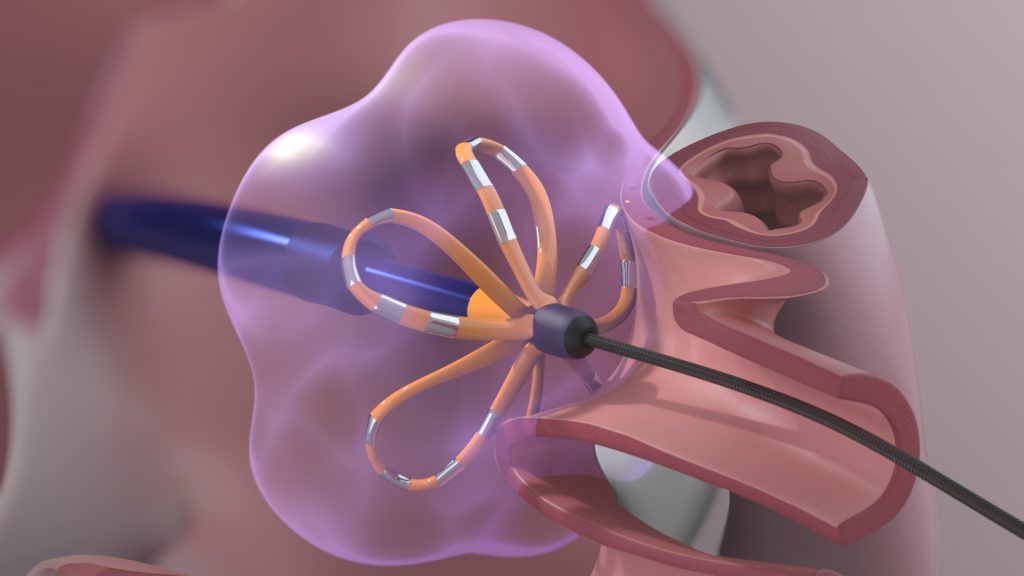
4. Left Atrial Appendage Closure (LAAC) – Watchman Device
For patients unable to tolerate blood thinners, the Watchman device offers an alternative to reduce stroke risk. It works by closing off the left atrial appendage (LAA), preventing blood clots from forming and potentially traveling to the brain.
- Procedure: The Watchman device is inserted through a catheter and placed in the LAA. Over time, tissue grows over the device, permanently sealing the LAA.
- Benefits: By closing the LAA, the Watchman device reduces stroke risk without the need for lifelong anticoagulation.
- Ideal Candidates: The device is often recommended for patients with a high risk of bleeding, those who have experienced complications with anticoagulants, or those with an active lifestyle incompatible with blood thinners.

For additional details on the Watchman device, visit our Watchman Device page.
5. Surgical Options: Maze Procedure
In some cases, minimally invasive surgery may be considered for AFib treatment. The Maze procedure is a surgical technique that creates a pattern of scar tissue in the atria, preventing the propagation of erratic electrical signals.
- Types of Maze Procedure: The traditional Maze procedure is open-heart surgery performed during other necessary heart surgeries, such as valve repair or bypass. There are also minimally invasive versions of the Maze procedure, performed through small incisions without the need for open-heart surgery.
- Considerations: The Maze procedure is typically reserved for patients who are already undergoing other cardiac surgeries or those who have not responded to other treatment methods.
6. Lifestyle Modifications
Lifestyle changes are essential for managing AFib and reducing its progression. These modifications can also improve the effectiveness of other treatments.
- Weight Management: Maintaining a healthy weight reduces the risk of AFib recurrence and improves overall heart health.
- Alcohol Reduction: Limiting or avoiding alcohol intake is essential, as alcohol can trigger AFib episodes.
- Regular Exercise: Moderate exercise helps maintain heart health, though intense physical exertion should be discussed with a healthcare provider.

- Diet: A heart-healthy diet, rich in fruits, vegetables, lean proteins, and whole grains, supports cardiovascular health.
- Sleep Apnea Management: Sleep apnea is a significant risk factor for AFib, and using a CPAP machine can reduce symptoms and AFib recurrence.

For more on lifestyle management and its impact on AFib, visit our page on Lifestyle and AFib.
Summary of AFib Treatment Options
The management of AFib requires a tailored approach, with options ranging from medications and lifestyle changes to advanced procedures like catheter ablation. Working with an electrophysiologist or cardiologist is essential to identify the most effective treatments for each patient’s unique needs.
- Medications: Blood thinners, rate control, and rhythm control medications are often the starting point.
- Procedures: Cardioversion, catheter ablation, and the Watchman device offer targeted interventions for rhythm control and stroke prevention.
- Surgical Options: The Maze procedure is available for certain cases.
- Lifestyle Modifications: Healthy lifestyle choices help prevent AFib progression and improve treatment success.
Through a combination of these treatments, patients with AFib can manage symptoms, reduce stroke risk, and improve their quality of life.
Section 6: AFib Ablation – A Closer Look at AFib Ablation Procedures
Atrial fibrillation ablation, commonly known as AFib ablation, is a minimally invasive procedure designed to treat AFib by targeting the areas in the heart responsible for abnormal electrical signals. AFib ablation is particularly useful for patients who have not responded well to medications or who wish to pursue a long-term solution for managing their AFib symptoms. This section will delve into the types of ablation techniques, procedure details, potential risks, benefits, and considerations for patients.
1. What is AFib Ablation?
AFib ablation is a procedure where the physician creates small scars in the heart tissue, typically around the pulmonary veins. These scars disrupt the erratic electrical signals causing AFib, helping to restore a normal heart rhythm.
The primary target in AFib ablation is the area where the pulmonary veins enter the left atrium. This location often produces the electrical impulses that trigger AFib episodes. By isolating or ablating these areas, the procedure aims to reduce or eliminate AFib episodes, improving the patient’s quality of life and decreasing the likelihood of symptom recurrence.
For more information, visit our page on What is AFib Ablation.
2. Types of AFib Ablation Techniques
There are multiple energy modalities used in AFib ablation, each with unique advantages. The choice of ablation method often depends on the patient’s specific AFib type, the physician’s expertise, and the availability of technology.
a. Radiofrequency (Thermal) Ablation
Radiofrequency ablation is the most common form of AFib ablation. It uses high-frequency electrical energy to heat and destroy the targeted heart tissue.
- Mechanism: The ablation catheter delivers radiofrequency energy to create lesions around the pulmonary veins, isolating the triggers of AFib.
- Benefits: Radiofrequency ablation has been studied extensively and shows high success rates for paroxysmal AFib.
- Considerations: Since this method uses heat, there is a slight risk of collateral damage to nearby structures, such as the esophagus.
b. Cryoablation (Cold) Ablation
Cryoablation uses extreme cold to create lesions in the heart tissue, freezing and eliminating abnormal pathways that contribute to AFib.
- Mechanism: A cryoballoon catheter is positioned in the pulmonary veins, delivering cold energy to freeze and isolate AFib triggers.
- Benefits: Cryoablation is quick and highly effective for paroxysmal AFib. It also has fewer risks of esophageal damage than radiofrequency ablation.
- Considerations: Cryoablation may be less suitable for complex cases, such as longstanding persistent AFib.
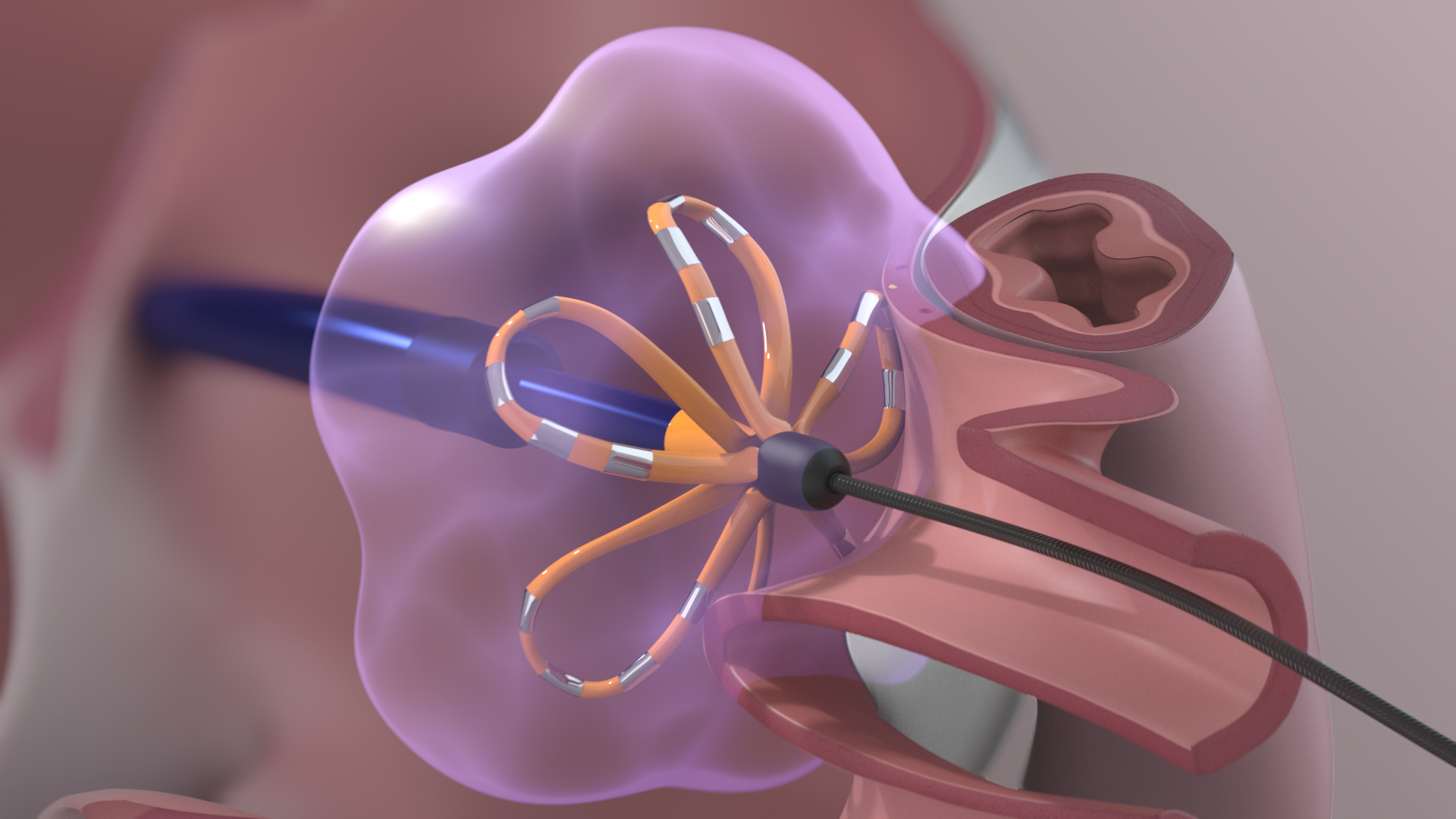
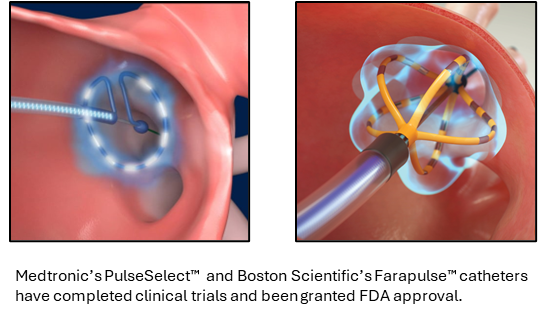
c. Pulsed Field Ablation (PFA)
Pulsed Field Ablation (PFA) is a newer technology using non-thermal electrical energy to ablate cardiac tissue.
- Mechanism: PFA delivers high-voltage electrical pulses that selectively target heart tissue without affecting surrounding structures like the esophagus and phrenic nerve.
- Benefits: Studies show that PFA is safer and faster than thermal ablation methods, with shorter procedure times and less risk of collateral damage.
- Availability: PFA is approved in Europe and is in advanced clinical trials in the U.S. Many experts believe it could become the standard for AFib ablation in the near future.
For more information, visit our Pulsed Field Ablation page.
3. The AFib Ablation Procedure
AFib ablation is typically performed under general anesthesia in a specialized electrophysiology (EP) lab. The procedure itself is minimally invasive and involves inserting catheters into the veins in the groin, which are then advanced to the heart.
- Preparation: Patients are sedated, and small punctures are made in the groin area to insert the catheters.
- Mapping: The physician uses a 3D mapping system to create a detailed image of the heart and locate the areas where abnormal signals originate.
- Ablation: Based on the type of ablation, the catheter delivers radiofrequency, cryo, or pulsed energy to the targeted heart tissue.
- Monitoring: The heart rhythm is monitored in real-time during the procedure to confirm the success of the ablation.
- Completion: Once all targeted areas are ablated, the catheters are removed, and the puncture sites are closed. Patients typically stay in the hospital for a night to monitor for any immediate complications.
4. Risks and Benefits of AFib Ablation
AFib ablation is generally safe, but as with any medical procedure, there are potential risks and benefits to consider.
Benefits
- Improved Quality of Life: Many patients experience a significant reduction in AFib symptoms, such as palpitations, fatigue, and breathlessness, following ablation.
- Reduced AFib Episodes: Ablation has been shown to reduce the frequency and severity of AFib episodes, particularly in patients with paroxysmal AFib.
- Minimized Need for Medications: Successful ablation may reduce or eliminate the need for antiarrhythmic drugs, which can have side effects and impact quality of life.
- Potential for Long-Term Success: Ablation can offer long-term success, especially when combined with lifestyle changes and other medical treatments.
Risks
- Bleeding and Infection: The risk of bleeding or infection at the catheter insertion site is minimal but present.
- Collateral Damage: Thermal ablation methods (radiofrequency and cryo) may affect nearby structures, though this risk is low with experienced practitioners.
- Arrhythmias: Some patients may experience new arrhythmias after ablation, but these are often temporary and resolve as the heart heals.
- Recurrence: While ablation is effective, AFib may recur in some patients, and repeat ablation may be necessary.
5. Success Rates and Follow-Up
The success rates of AFib ablation vary depending on factors such as the type of AFib, patient health, and the experience of the physician and facility performing the procedure. In general, success rates are highest in patients with paroxysmal AFib (75–90%) and lower for those with persistent or longstanding AFib. For patients with recurrent episodes, repeat ablation can often enhance long-term outcomes.
Follow-Up After Ablation
Post-ablation follow-up is essential to monitor heart rhythm and ensure the long-term success of the procedure. A typical follow-up schedule includes:
- Initial Monitoring: An ECG and wearable heart monitor may be used to check for any early recurrence of AFib in the weeks following ablation.
- Routine Check-Ups: Regular appointments with a cardiologist or electrophysiologist will help monitor heart health and assess the need for any additional interventions.
- Medication Review: Some patients may be able to reduce or discontinue certain medications, like antiarrhythmics, following a successful ablation.
- Lifestyle Recommendations: Patients are encouraged to continue with lifestyle modifications, such as weight management and exercise, to improve long-term outcomes.
For more information on life after AFib ablation, visit our AFib Ablation Follow-Up page.
6. Lifestyle Changes to Support AFib Ablation Success
Lifestyle modifications play a crucial role in ensuring long-term success following AFib ablation. Maintaining a healthy lifestyle can reduce the risk of AFib recurrence and enhance overall heart health:
- Weight Management: Aim to maintain a healthy BMI, as excess weight increases the risk of AFib recurrence.
- Moderate Exercise: Incorporate regular, moderate exercise while avoiding high-intensity activities that may trigger AFib episodes.
- Limit Alcohol Intake: Alcohol can trigger AFib, so it’s best to consume it in moderation.
- Quit Smoking: Smoking cessation is essential for heart health and reducing AFib recurrence.
For more information on lifestyle tips, visit our section on Lifestyle Modifications for AFib.
Pulsed Field Ablation: A New Frontier in AFib Treatment
Pulsed Field Ablation (PFA) represents a transformative step forward in the treatment of atrial fibrillation (AFib), offering a unique, non-thermal approach to ablation. Traditional ablation methods, which rely on radiofrequency (heating) or cryotherapy (cooling), carry a risk of collateral damage to nearby structures. PFA, by contrast, uses precisely controlled electrical pulses, creating selective lesions in the heart tissue without the thermal impact that can harm adjacent structures like the esophagus, nerves, or blood vessels. This novel technique has already shown promising safety and efficacy profiles and is positioned to become a new standard in AFib ablation.
What Is Pulsed Field Ablation?
Pulsed Field Ablation utilizes a technology called electroporation, where high-voltage electric pulses create microscopic pores in cell membranes, leading to cell death in a controlled and targeted manner. In PFA for AFib, these pulses are applied specifically to cardiac tissue to disrupt abnormal electrical pathways that cause the atrial fibrillation. Importantly, PFA’s non-thermal nature reduces the risk of unintentional damage to surrounding tissues, making it a safer alternative for AFib ablation.
For a deeper understanding, explore the What Is Pulsed Field Ablation? page on our website.
Advantages of Pulsed Field Ablation Compared to Traditional Methods
1. Selective Tissue Targeting
- PFA is cardio-selective, meaning it affects only cardiac cells at the voltage levels applied. Adjacent structures like the esophagus, vagus nerve, and pulmonary veins, which can be at risk during thermal ablations, are typically unaffected. This selectivity significantly reduces the potential for complications and long-term side effects.
2. Enhanced Safety Profile
- Unlike radiofrequency and cryoablation, which can cause complications due to extreme heat or cold, PFA reduces the risk of injury to non-cardiac tissues, particularly the esophagus. PFA’s safety profile makes it an attractive option, especially for patients with anatomical considerations that make thermal ablation more risky.
3. Shorter Procedure Times
- PFA generally requires less time in the EP lab, as the energy delivery is rapid and precise. Shorter procedures reduce anesthesia time and allow more patients to be treated, which is especially beneficial in busy medical centers.
4. Improved Procedure Outcomes
- Initial studies and real-world applications in Europe have shown that PFA is at least as effective as traditional methods in treating AFib, with fewer complications and a shorter recovery time. This increased safety and efficacy make it an option for more AFib patients.
The PFA Procedure: What to Expect
The PFA procedure follows a similar process to other catheter-based ablations:
- Preparation: Patients are given either conscious sedation or general anesthesia.
- Catheter Insertion: A catheter is inserted through a small incision, typically in the groin, and guided to the heart using advanced imaging.
- Energy Delivery: Once positioned near the pulmonary veins and other AFib-triggering areas, the catheter delivers a series of controlled electrical pulses to create precise lesions.
- Recovery: After the ablation, patients are monitored and usually discharged within 24 hours.
Explore our Pulsed Field Ablation Treatment Overview for more on the procedure and patient experiences.
Who Can Benefit from Pulsed Field Ablation?
Pulsed Field Ablation may be particularly beneficial for:
- Patients at risk of complications from thermal ablation: Due to the selective nature of PFA, patients with anatomical risks may have a safer experience.
- Recurrent AFib patients: Those with persistent or recurrent AFib episodes who have not responded to medication or previous ablation methods.
- Patients seeking a shorter recovery time: PFA’s efficiency reduces recovery time, making it suitable for patients looking to resume normal activities quickly.
Future Outlook of Pulsed Field Ablation
While PFA is relatively new, the success rates and safety profiles seen in Europe are encouraging. As more clinical data becomes available in the U.S., and with the ongoing adoption of PFA in specialized centers, this method has the potential to redefine how AFib ablation is performed. Innovations in catheter design and procedural techniques may further enhance PFA’s efficacy and expand its application.
At The AFib Clinic, we are at the forefront of integrating advanced treatments like Pulsed Field Ablation to improve patient outcomes. Dr. Jose Osorio and his team are experienced in both traditional and novel ablation techniques, offering patients a comprehensive approach to managing AFib effectively.
Comparing AFib Ablation Techniques: Radiofrequency, Cryoablation, and Pulsed Field Ablation
Atrial Fibrillation (AFib) ablation is a key treatment for managing this arrhythmia, particularly for those whose symptoms impact their quality of life. Over the years, multiple ablation techniques have been developed to target and eliminate the tissue causing AFib, each with unique methods and benefits. This section explores the three primary techniques—Radiofrequency Ablation, Cryoablation, and the novel Pulsed Field Ablation (PFA)—and compares their safety, efficacy, and patient experience.
1. Radiofrequency Ablation (RFA)
Radiofrequency Ablation (RFA) uses heat generated by radio waves to create precise lesions in the heart tissue, particularly around the pulmonary veins. This heating process disrupts the electrical pathways responsible for AFib, effectively “disconnecting” the areas that trigger irregular heart rhythms.
- Procedure: A catheter is inserted into a vein, usually in the groin, and guided to the heart. Once positioned, radiofrequency energy is delivered, heating the tissue to create lesions.
- Advantages:
- Extensive use with well-documented outcomes over decades of clinical practice.
- Effective for patients with both paroxysmal (intermittent) and persistent AFib.
- Risks:
- Collateral damage to adjacent structures, such as the esophagus or nerves, due to heat transfer.
- Risk of blood clot formation, potentially leading to stroke if not managed properly.
2. Cryoablation
Cryoablation is another commonly used ablation technique that uses extreme cold to freeze and isolate the tissue triggering AFib, particularly around the pulmonary veins. The process involves cooling the tissue to a point where it becomes non-functional, effectively blocking the erratic electrical signals causing AFib.
- Procedure: Similar to radiofrequency ablation, a catheter is inserted and guided to the target area. Instead of heat, a cryoballoon is used to deliver freezing temperatures to ablate the tissue surrounding the pulmonary veins.
- Advantages:
- Provides uniform lesion formation with the cryoballoon technique, reducing procedural complexity.
- Often faster than radiofrequency ablation, with minimal or no use of fluoroscopy (X-ray) for guidance.
- Risks:
- Potential damage to nearby tissues, such as the phrenic nerve, which could result in temporary or long-term breathing difficulties.
- Lower success rates compared to some radiofrequency techniques in certain patient groups, such as those with persistent AFib.
To read more about cryoablation and its specific applications, explore Cryoballoon Ablation Technique.
3. Pulsed Field Ablation (PFA)
Pulsed Field Ablation is a newer, non-thermal approach that uses short electrical pulses instead of heat or cold to ablate cardiac tissue. This selective technique affects only the targeted heart tissue without damaging nearby structures, making it a promising alternative to traditional methods.
- Procedure: High-voltage electrical pulses are delivered in brief bursts, creating a field that alters the cellular structure of the targeted heart tissue. This technique, known as irreversible electroporation, allows for precise ablation with minimal collateral damage.
- Advantages:
- Cardio-selective: Minimizes risks to nearby structures, such as the esophagus and nerves, providing a safer profile for patients.
- Shorter procedural times and reduced need for anesthesia, making it less taxing for patients and operators alike.
- A promising technique for patients with paroxysmal AFib and those who may not be suitable for other ablation types.
- Risks:
- Limited long-term data as the technology is newer, though early studies show high safety and efficacy.
- Potential for procedural learning curve, as widespread adoption and experience with PFA grow.
For more details on how PFA is transforming AFib treatment, visit Pulsed Field Ablation Overview.
Comparative Analysis
| Technique | Mechanism | Procedure Time | Risks | Benefits |
|---|---|---|---|---|
| Radiofrequency | Heat | Moderate | Esophageal and nerve injury | Well-documented, effective |
| Cryoablation | Cold | Shorter | Phrenic nerve damage | Uniform lesion formation |
| Pulsed Field Ablation | Electrical pulses | Shortest | Limited long-term data, minor learning curve | Safe for surrounding tissues |
Conclusion
Each ablation technique has unique strengths and limitations, with RFA and cryoablation offering established, effective options and PFA emerging as a promising safer alternative. Selecting the best approach depends on each patient’s unique clinical profile, AFib type, and overall health goals.
Procedure Preparation and Recovery for AFib Treatments
Preparing for AFib Treatment Procedures Preparation for an AFib treatment procedure—whether it’s ablation, left atrial appendage closure with the Watchman device, or cardioversion—requires a collaborative approach between the patient and healthcare team. Proper preparation can improve procedural success, minimize risks, and support a smoother recovery.
- Medical Evaluation and Tests:
- Pre-procedure Evaluation: Patients will undergo a thorough evaluation that includes an ECG, echocardiogram, and possibly blood work to check for clotting, kidney function, and other relevant parameters.
- Imaging: Sometimes, a transesophageal echocardiogram (TEE) may be recommended to check for clots in the heart before ablation.
- Medication Adjustments: Blood thinners and antiarrhythmic medications may need adjustment before the procedure. For example, anticoagulants like warfarin or direct oral anticoagulants (DOACs) may be paused or continued based on the type of AFib treatment planned.
- Pre-procedure Guidelines:
- Fasting: Patients are generally asked to fast for at least 6–8 hours before the procedure to reduce aspiration risk during anesthesia.
- Hydration: Adequate hydration before fasting is often encouraged to prevent dehydration, especially if diuretics or other medications are in use.
- Personal Arrangements: Since most procedures require sedation or anesthesia, patients should arrange for someone to drive them home and to assist for at least the first 24 hours post-procedure.
- Mental Preparation:
- It’s common for patients to experience anxiety before any heart-related procedure. Practicing relaxation techniques, deep breathing exercises, or even consulting with a counselor or support group may provide relief.
What to Expect on the Day of the Procedure
- Admission and Pre-Procedure Setup:
- Patients will check in and change into hospital attire. A nurse or technician will insert an intravenous (IV) line for medications, fluids, and anesthesia.
- The healthcare team will conduct a final review of the patient’s medical history, confirm consent, and answer any last-minute questions.
- Anesthesia:
- Most AFib procedures, such as ablation and the Watchman device implantation, are done under conscious sedation or general anesthesia. This ensures comfort throughout the procedure.
- During the Procedure:
- Catheter Ablation: The electrophysiologist will insert catheters through a vein in the groin and guide them to the heart. Using imaging and specialized mapping systems, they will locate and treat areas responsible for AFib.
- Left Atrial Appendage Closure: For the Watchman device, the device is guided to the left atrial appendage, where it is deployed to block clot formation.
- Cardioversion: A quick and straightforward procedure, cardioversion involves using electrical energy to reset the heart rhythm to normal, often with mild anesthesia for patient comfort.
Recovery After AFib Procedures
- Immediate Post-Procedure Care:
- Observation: Patients typically spend several hours in a recovery area, where their vital signs and heart rhythm are monitored. Some may stay overnight, especially if it was an ablation or left atrial appendage closure.
- Pain Management: Mild discomfort, particularly at the catheter insertion site, is common. Pain medications may be provided, but significant pain is rare.
- Returning Home:
- Most patients can go home within 24 hours of the procedure, although they should refrain from strenuous activity for about a week.
- Incision Care: Patients are advised to keep the insertion site clean and dry. Bruising is normal, but any signs of infection—such as redness, swelling, or fever—should be reported.
- Resuming Activities:
- Physical Activity: Walking and light activity are encouraged soon after the procedure to prevent blood clots, but heavy lifting and intense physical activity should be avoided for at least a week.
- Medications: Blood thinners may be resumed post-procedure, and new prescriptions may be provided based on individual needs. For example, after an ablation, antiarrhythmic drugs might be temporarily continued to support rhythm stability.
- Follow-Up Appointments:
- Follow-up visits with an electrophysiologist are typically scheduled within one to two weeks post-procedure. Regular follow-ups may continue to monitor for AFib recurrence, medication effectiveness, and overall heart health.
- Monitoring and Long-Term Recovery:
- Some patients may be advised to use at-home monitors, such as wearable ECG devices, to detect any recurrence of AFib.
- Patients are encouraged to continue lifestyle modifications to support long-term heart health, including managing weight, blood pressure, and avoiding AFib triggers.
Tips for a Smooth Recovery and Maintaining Heart Health
- Hydrate and Nourish: Proper hydration and a heart-healthy diet are essential for healing.
- Avoid Stimulants: Stimulants like caffeine or alcohol can trigger irregular rhythms and should be limited or avoided, especially in the early recovery phase.
- Stress Management: Managing stress through relaxation techniques, mindfulness, and exercise can contribute to a healthier heart rhythm.
- Know When to Seek Help: Patients should contact their healthcare team if they experience severe symptoms, such as chest pain, shortness of breath, or swelling, or if they notice AFib symptoms returning.
With careful preparation, an understanding of what to expect, and attentive post-procedure care, AFib patients can achieve successful treatment outcomes and improved quality of life. For further guidance on preparing for specific AFib procedures, please refer to the detailed sections on AFib Treatment Options and Procedure Preparation on our website.
Section 7: Stroke Risk and Prevention in AFib Patients
Stroke is one of the most significant risks for patients with Atrial Fibrillation (AFib), as AFib increases the likelihood of stroke by up to five times. In AFib, the upper chambers of the heart (atria) don’t contract effectively, causing blood to pool and increasing the risk of clot formation. When these clots travel through the bloodstream, they can block an artery in the brain, resulting in a stroke. Understanding and managing stroke risk is a critical component of AFib treatment, with strategies that include stroke risk assessment tools, anticoagulant medications, and procedures like the Watchman device for left atrial appendage closure.
Understanding Stroke Risk in AFib
The increased risk of stroke in AFib patients comes from the irregular quivering of the atria, which prevents efficient blood flow and can lead to clot formation. Most blood clots in AFib patients develop in a small pouch of the heart known as the left atrial appendage (LAA). To manage this risk effectively, AFib patients undergo a personalized stroke risk assessment.
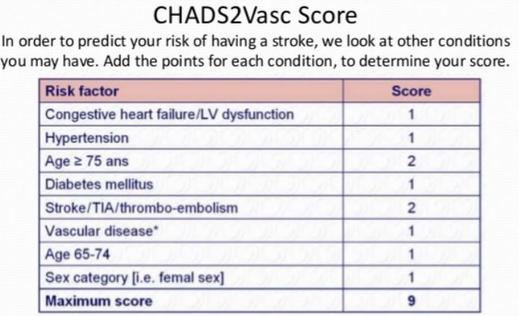
The CHADS2-VASc Score
The CHADS2-VASc score is a tool commonly used by physicians to evaluate an individual’s annual stroke risk. By adding points for specific conditions, such as heart failure, hypertension, age, diabetes, and vascular disease, physicians determine the necessity of stroke prevention measures like blood thinners.
The components of the CHADS2-VASc scoring system include:
- C: Congestive Heart Failure (+1 point)
- H: Hypertension (+1 point)
- A: Age 75 or older (+2 points)
- D: Diabetes Mellitus (+1 point)
- S2: Prior Stroke or Transient Ischemic Attack (TIA) (+2 points)
- V: Vascular Disease (+1 point)
- A: Age 65-74 (+1 point)
- Sc: Sex Category (Female = +1 point)
The higher the score, the greater the annual risk of stroke, guiding treatment plans focused on stroke prevention.
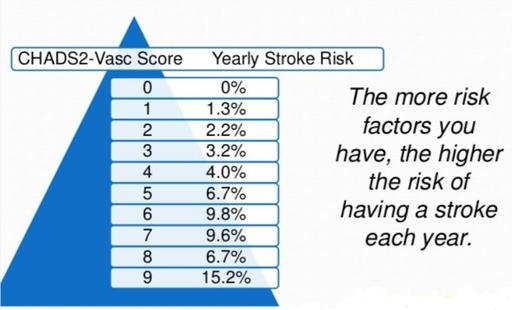
For more information on how stroke risk is assessed, visit our Stroke Risk for Patients with AFib page.
Stroke Prevention Strategies
Once stroke risk is assessed, there are several approaches to reducing the risk. The main treatment options include anticoagulant medications, lifestyle modifications, and procedural interventions.
1. Blood Thinners (Anticoagulants)
Anticoagulants, or blood thinners, are the first line of defense for reducing stroke risk in AFib patients. They work by decreasing the blood’s ability to clot, thus reducing the likelihood of clots forming in the left atrium and moving to the brain.
- Direct Oral Anticoagulants (DOACs): DOACs, such as apixaban (Eliquis), rivaroxaban (Xarelto), and dabigatran (Pradaxa), are newer anticoagulants that don’t require regular blood tests or dietary restrictions.
- Warfarin (Coumadin): Warfarin has been used for decades, but it requires frequent INR monitoring and dietary management to maintain the appropriate therapeutic range.
- Risk-Benefit Balance: Anticoagulants effectively reduce stroke risk but carry a risk of bleeding. The HAS-BLED score is another tool used by physicians to evaluate the bleeding risk associated with anticoagulant therapy, ensuring that the benefits of stroke prevention outweigh the risks.
For further details on blood thinners, please check out our Common AFib Medications page.
2. Left Atrial Appendage Closure: The Watchman Device
In patients with a high risk of bleeding or those who cannot take blood thinners long-term, left atrial appendage closure is an alternative to reduce stroke risk. The Watchman device is designed to seal off the LAA, preventing clots from forming in this area and reducing stroke risk.
- Procedure: The Watchman device is inserted through a catheter into the left atrium, where it seals off the LAA. Over time, heart tissue grows over the device, permanently closing off the appendage.
- Benefits: The Watchman procedure reduces stroke risk without the need for lifelong anticoagulants, making it an ideal option for patients at high risk of bleeding or those with active lifestyles that make blood thinners challenging.
For more information, visit our Watchman Device page.
Lifestyle Modifications for Stroke Prevention
Beyond medications and procedures, certain lifestyle changes can help reduce stroke risk for AFib patients. These modifications also help manage overall heart health, providing additional benefits for AFib management and prevention.
1. Blood Pressure Management
- Hypertension is a significant risk factor for stroke, especially in AFib patients. Lifestyle changes such as a heart-healthy diet, regular exercise, and reducing salt intake can lower blood pressure and minimize stroke risk.
- For those requiring medication, a physician may prescribe antihypertensive drugs to keep blood pressure under control.
2. Diabetes and Blood Sugar Control
- Diabetes increases the risk of stroke and worsens AFib outcomes. Maintaining blood sugar levels through diet, exercise, and medication (when necessary) helps minimize stroke risk and manage AFib.
3. Weight Management
- Obesity is linked to both AFib and increased stroke risk. Weight loss through diet, exercise, and, if appropriate, medications like GLP-1 agonists (e.g., Wegovy or Mounjaro) can reduce stroke risk and improve heart health overall.
4. Reducing Alcohol and Smoking
- Alcohol and smoking are both known risk factors for stroke and worsen AFib. Minimizing alcohol consumption and quitting smoking can reduce stroke risk while also benefiting heart health.
5. Physical Activity
- Regular physical activity, such as walking or cycling, helps maintain a healthy heart and vascular system, reducing stroke risk in AFib patients. However, it’s essential to tailor exercise intensity to each patient’s condition and to avoid overexertion, which can sometimes trigger AFib episodes.
6. Treating Obstructive Sleep Apnea (OSA)
- Sleep apnea is strongly associated with AFib and stroke. Treating OSA with CPAP (Continuous Positive Airway Pressure) therapy has been shown to reduce AFib episodes and may lower stroke risk.
For more detailed information on lifestyle changes for stroke prevention in AFib, visit our AFib and Lifestyle page.
Additional Considerations for Stroke Prevention
Regular Monitoring and Follow-Up
- Ongoing assessment of stroke risk and bleeding risk is essential, particularly for patients on anticoagulant therapy. Regular follow-up appointments with a cardiologist or electrophysiologist ensure that the chosen treatment strategy remains appropriate and effective.
Patient Education and Symptom Awareness
- Educating patients about the symptoms of stroke—such as sudden numbness, confusion, trouble speaking, or loss of balance—is critical. Prompt recognition and treatment are crucial in minimizing the long-term impact of a stroke.
- AFib patients should also be aware of AFib triggers, such as stress, dehydration, or certain foods, which could lead to an AFib episode that increases stroke risk.
Wearable Technology for Monitoring
- Devices like the Apple Watch can monitor heart rhythms and alert patients to possible AFib episodes. While not a replacement for medical monitoring, these wearables offer an added layer of protection, allowing patients to seek medical attention if AFib episodes increase.
For more on wearable technology and AFib monitoring, see our Apple Watch and AFib page.
Summary of Stroke Prevention in AFib
In AFib management, stroke prevention is of utmost importance. By combining anticoagulant medications, lifestyle changes, procedural interventions like the Watchman device, and continuous monitoring, patients can significantly reduce their risk of stroke and improve their quality of life. Each patient’s treatment plan is individualized based on their specific risk factors, making it essential to work closely with a healthcare provider for optimal management.
- Anticoagulants: Primary choice for stroke prevention but may carry bleeding risks.
- Left Atrial Appendage Closure: Alternative for patients who cannot tolerate anticoagulants.
- Lifestyle Modifications: Control of blood pressure, weight, diabetes, and habits like smoking and alcohol consumption.
- Monitoring and Technology: Regular follow-ups and wearable technology for ongoing rhythm and symptom monitoring.
Effective stroke prevention combines medical interventions, lifestyle adjustments, and a proactive approach to patient care, ensuring the best possible outcomes for AFib patients.
Section 8: Conditions That Cause or Worsen AFib: Sleep Apnea, Obesity, Hypertension, and Alcohol
AFib is often associated with other health conditions that can either trigger the onset of arrhythmias or exacerbate existing AFib episodes. Understanding and managing these contributing factors is essential for patients seeking to reduce AFib frequency, severity, and progression. This section provides an in-depth look at some of the most common conditions linked to AFib: Sleep Apnea, Obesity, Hypertension, and Alcohol Consumption.
Sleep Apnea and AFib
Sleep apnea, particularly Obstructive Sleep Apnea (OSA), has a well-documented relationship with AFib. OSA is a disorder where the airway becomes temporarily blocked during sleep, causing repeated breathing interruptions. These interruptions cause fluctuations in blood oxygen levels, increasing the workload on the heart and promoting an environment conducive to AFib.
- Mechanism of Impact: During an apnea episode, oxygen levels drop, and the body responds by releasing stress hormones, which raise blood pressure and can alter heart function. Over time, these factors can lead to atrial enlargement and remodeling, increasing AFib risk.
- Treatment: The primary treatment for OSA is Continuous Positive Airway Pressure (CPAP) therapy, which helps keep the airway open during sleep. Studies have shown that CPAP therapy can significantly reduce AFib episodes and improve outcomes in patients who undergo AFib ablation. Weight loss and lifestyle changes can further reduce the impact of sleep apnea on AFib.
- For more information on the connection between sleep apnea and AFib, visit our detailed page on AFib and Sleep Apnea.

Obesity and AFib
Obesity is a significant risk factor for developing AFib and can make existing AFib more difficult to manage. Excess body weight strains the heart, alters its structure, and leads to inflammation, all of which can contribute to AFib.
- Mechanism of Impact: Obesity is associated with atrial enlargement and ventricular hypertrophy, which contribute to electrical disturbances in the heart. Additionally, obesity increases the risk of other conditions such as hypertension and diabetes, which further increase AFib risk.
- Weight Loss Benefits: Weight loss has been shown to reduce AFib frequency, lower the burden of AFib, and improve treatment outcomes, including the success rate of ablation procedures. In some cases, GLP-1 receptor agonists, such as Wegovy, can aid in weight loss, particularly in patients who struggle with traditional methods.
- Visit our page on Weight Loss and AFib to learn more about how obesity influences AFib and available treatment options.
Hypertension and AFib
Hypertension (high blood pressure) is a primary contributor to AFib, and managing blood pressure is critical to reducing AFib’s effects. Elevated blood pressure can lead to structural changes in the heart and increase the risk of heart failure, both of which are closely linked to AFib.
- Mechanism of Impact: High blood pressure causes the heart to work harder to pump blood, leading to left ventricular hypertrophy and atrial remodeling. These changes in the heart’s structure can disrupt electrical signaling and promote AFib.
- Management: Effective blood pressure management through lifestyle changes and medication is essential for AFib patients. Reducing sodium intake, managing stress, and increasing physical activity are all helpful lifestyle modifications. Certain antihypertensive medications can also help control AFib symptoms, particularly those that target heart rate and rhythm.
- For more details on hypertension and its relationship with AFib, refer to our comprehensive page on Hypertension and AFib.
Alcohol Consumption and AFib
Alcohol is a common AFib trigger, with even moderate drinking capable of increasing AFib episodes in some individuals. Known as “Holiday Heart Syndrome”, alcohol-related AFib episodes are especially common after heavy drinking.
- Mechanism of Impact: Alcohol affects the heart by disrupting its electrical pathways and promoting structural changes over time, particularly when consumed in high amounts. Additionally, alcohol can trigger a stress response in the body, leading to elevated blood pressure and irregular heart rhythms.
- Recommendations: Limiting or avoiding alcohol can reduce AFib frequency. Some patients find that even small amounts of alcohol can trigger symptoms, while others may tolerate moderate intake. It’s important to identify individual sensitivities and adjust consumption accordingly.
- For a deeper dive into how alcohol affects AFib, read our article on Alcohol and AFib.
Other Lifestyle Factors
In addition to these conditions, other lifestyle factors can also influence AFib:
- Smoking: Smoking damages blood vessels, raises blood pressure, and promotes atherosclerosis, all of which contribute to AFib. Quitting smoking has significant benefits for both heart health and AFib management.
- Physical Inactivity: A sedentary lifestyle increases AFib risk. Regular moderate exercise can help manage AFib by improving cardiovascular health, promoting weight loss, and reducing blood pressure.
- Stress and Anxiety: Stress can elevate heart rate and lead to AFib episodes. Techniques such as meditation, yoga, and mindfulness may help reduce stress-related AFib triggers.
These lifestyle factors play a critical role in both the onset and management of AFib. Patients are encouraged to make healthy lifestyle choices to maximize the effectiveness of any medical treatments and improve their overall heart health.
Explore Related Resources
To learn more about these conditions and AFib management, please visit:
New Developments in Weight Loss Drugs for AFib Patients
Overview of Weight Loss in AFib Management Weight management is crucial for managing atrial fibrillation (AFib) since excess weight is a known risk factor. Obesity can increase the heart’s workload and raise the risk of conditions like hypertension and sleep apnea, all of which can worsen AFib symptoms or frequency. Recent advancements in weight-loss medications, especially GLP-1 agonists, are offering new, effective options for patients who struggle with traditional weight-loss methods.
The Role of Weight Loss Drugs in AFib For patients with AFib, achieving and maintaining a healthy weight can help reduce AFib episodes and improve overall heart health. Traditional methods of weight management—diet, exercise, and sometimes surgery—are still foundational. However, medications like Wegovy, Mounjaro, and Zepbound, known as GLP-1 agonists, are now showing promise in helping patients lose significant weight without invasive procedures.
How GLP-1 Agonists Work GLP-1 (glucagon-like peptide-1) agonists mimic a hormone in the body that affects hunger and fullness. By stimulating receptors in the brain that signal satiety, GLP-1 agonists reduce appetite, helping individuals consume fewer calories. This class of medications includes semaglutide (used in Wegovy) and tirzepatide (found in Mounjaro). In clinical trials, these drugs have shown an average weight loss of 15–20% over one to two years, which is significant for heart health.
The Potential Benefits for AFib Patients In addition to weight loss, GLP-1 agonists have other heart-health benefits:
- Reduced Blood Pressure and Inflammation: GLP-1 agonists may improve blood pressure control and have mild anti-inflammatory effects, which benefit overall cardiovascular health.
- Improved Blood Sugar Control: These drugs are especially beneficial for AFib patients with diabetes, as they help regulate blood sugar, further supporting heart function.
Considerations and Risks While promising, GLP-1 agonists have limitations:
- Side Effects: Common side effects include nausea, vomiting, and, in some cases, more severe conditions like gallbladder disease.
- Long-Term Use and Costs: These medications need to be taken continuously to maintain their weight-loss effects, and discontinuing them often leads to weight regain.
- Individual Variation: Not every patient responds equally to GLP-1 agonists, and their effectiveness may vary.
For AFib patients considering weight-loss medication, consulting with a cardiologist and an endocrinologist is essential to weigh the benefits against potential risks.
Living with AFib: Long-Term Management and Prognosis
Managing atrial fibrillation (AFib) effectively over the long term requires a combination of medical treatment, lifestyle changes, and regular follow-up with healthcare providers. While AFib may be a chronic condition, many patients lead full, active lives with the proper management plan. This section explores essential aspects of long-term AFib management, from medication adherence to lifestyle adjustments and regular monitoring, to enhance both quality of life and prognosis.
1. Understanding the Long-Term Goals in AFib Management
- Stroke Prevention: Since AFib significantly increases the risk of stroke, the primary goal is to manage this risk through blood thinners, lifestyle modifications, and, in some cases, procedures like left atrial appendage closure (Watchman device).
- Symptom Control: Managing symptoms such as palpitations, dizziness, and fatigue is vital to improving quality of life. This may involve a combination of rate or rhythm control medications and regular monitoring to adjust treatments as needed.
- Disease Progression Prevention: AFib tends to progress from paroxysmal (occasional) to persistent and, ultimately, permanent. Early intervention with lifestyle changes, medications, or ablation can slow this progression and improve outcomes.
2. Medication Adherence and Regular Review
- Blood Thinners: Patients at high risk of stroke, as determined by their CHA₂DS₂-VASc score, are typically prescribed blood thinners like warfarin, apixaban, or rivaroxaban. Long-term adherence is critical, and regular follow-up with blood work (if on warfarin) ensures safe and effective dosing.
- Rate and Rhythm Control: Medications such as beta-blockers, calcium channel blockers, and antiarrhythmic drugs are used to manage heart rate and rhythm. Periodic ECGs help monitor the effectiveness of these medications, with adjustments made as necessary based on symptoms and heart rate.
- Monitoring for Side Effects: Blood thinners and certain antiarrhythmic drugs may increase the risk of side effects, including bleeding or dizziness. Regular check-ins with healthcare providers can help identify these early and make necessary changes.
3. Lifestyle Modifications for Long-Term Health
- Diet and Nutrition: A heart-healthy diet rich in vegetables, fruits, whole grains, lean proteins, and low in sodium and unhealthy fats helps manage weight, blood pressure, and overall cardiovascular health. Reducing alcohol intake is also beneficial, as it can be an AFib trigger.
- Exercise: Moderate exercise is encouraged for most patients, but intense exercise should be approached cautiously and discussed with a healthcare provider. Activities like walking, swimming, or biking can improve cardiovascular fitness without overtaxing the heart.
- Weight Management: Maintaining a healthy weight is crucial as excess body weight can worsen AFib and reduce the success rate of treatments like ablation. GLP-1 agonists, such as Wegovy or Ozempic, are an option for some AFib patients needing weight management and can be discussed with a doctor.
- Sleep Hygiene: Poor sleep and conditions like obstructive sleep apnea are strongly linked to AFib. Ensuring good sleep hygiene and, if necessary, using CPAP therapy for sleep apnea can reduce AFib recurrence.
- Stress Management: Chronic stress can be a trigger for AFib. Practices like yoga, meditation, and mindfulness can help manage stress levels, reducing AFib frequency for some patients.
4. Regular Monitoring and Follow-Up Appointments
- Scheduled Check-Ins: Patients with AFib should have regular appointments with their cardiologist or electrophysiologist to review symptoms, medication efficacy, and overall heart health. During these visits, doctors may adjust medications, assess the need for further treatments, and monitor risk factors like blood pressure and cholesterol.
- Wearable Technology: Devices such as the Apple Watch or other ECG-equipped wearables are helpful tools for monitoring heart rhythm in real time. Wearables can help track AFib episodes and alert patients to irregular rhythms, enabling them to seek timely medical advice.
- Blood Pressure Monitoring: High blood pressure is a key risk factor for AFib and stroke. Regular home monitoring of blood pressure allows patients to track their levels and adjust lifestyle or medications as needed.
5. Understanding the Prognosis for AFib Patients
- Risk of Complications: AFib increases the risk of stroke, heart failure, and other cardiovascular complications. However, with proper management, including blood thinners, lifestyle adjustments, and possibly ablation, many patients significantly reduce these risks.
- Long-Term Management for Different Types of AFib: Prognosis depends on the AFib type (paroxysmal, persistent, or permanent). Earlier intervention generally leads to better outcomes, so consistent monitoring and management are crucial.
- Living a Full Life with AFib: With a proactive approach to health, many patients with AFib lead long, fulfilling lives. Effective AFib management involves ongoing collaboration with healthcare providers, making informed lifestyle choices, and remaining vigilant with follow-up care.
Resources for Further Learning and Support
- The AFib Clinic’s Overview on Lifestyle Changes for AFib Management
- Stroke Prevention Options in AFib Patients
- Monitoring AFib with Wearables
With careful adherence to prescribed treatments and lifestyle adjustments, individuals with AFib can reduce the risk of complications, improve their quality of life, and better manage their long-term prognosis.
Section 9: Frequently Asked Questions about AFib
This FAQ section provides answers to some of the most common questions about atrial fibrillation (AFib), drawing on essential topics covered throughout this guide. For further details, you can also explore the in-depth resources provided at The AFib Clinic’s Website.
1. What is Atrial Fibrillation (AFib)?
Atrial fibrillation is a heart rhythm disorder where the upper chambers of the heart (the atria) beat irregularly and rapidly. This irregular rhythm can lead to symptoms like heart palpitations, dizziness, and fatigue and significantly increases the risk of stroke. You can learn more about AFib on our What is AFib page.
2. What causes AFib?
AFib can result from various factors, including high blood pressure, heart disease, obesity, sleep apnea, and even lifestyle choices such as excessive alcohol intake or smoking. Some individuals also have a genetic predisposition to AFib. For more information, visit our AFib Overview page.
3. How is Afib diagnosed?
AFib is typically diagnosed using an electrocardiogram (ECG) or other heart rhythm monitoring devices. This can sometimes be a challenge with paroxysmal (intermittent) AFib, where additional monitoring techniques, such as Holter monitors or implantable loop recorders, may be used. Visit our AFib Diagnosis page for more details.
4. What are the symptoms of AFib?
Common symptoms include heart palpitations, an irregular heartbeat, chest pain, fatigue, dizziness, and shortness of breath. Some people may not experience any symptoms, making regular monitoring crucial for those at risk. Learn more on our Symptoms of AFib page.
5. What are the risks of untreated AFib?
Untreated AFib can lead to serious complications, including stroke, heart failure, and an overall decline in quality of life. Regular monitoring and timely treatment can help reduce these risks significantly. For more on treatment strategies, visit our AFib Treatment Options page.
6. How is AFib treated?
AFib treatment may include lifestyle changes, medications (for rate and rhythm control or stroke prevention), and procedures like AFib ablation. Treatment plans are customized to each patient’s unique needs and goals. Explore all available treatment options on our AFib Treatment Options page.
7. Can AFib go away on its own?
While some paroxysmal AFib episodes can stop without intervention, most patients experience recurring episodes. Over time, these episodes tend to increase in frequency and duration. Learn more about the chronic nature of AFib on our Does AFib Go Away? page.
8. Is AFib a lifelong condition?
For many, AFib is a chronic condition. However, with effective management, patients can lead fulfilling lives and often see a reduction in symptoms and complications. Read more about long-term AFib management on our Living with AFib page.
9. What is the difference between AFib and a heart attack?
AFib is an electrical problem causing an irregular heartbeat, while a heart attack occurs when blood flow to part of the heart is blocked. Both conditions require immediate medical attention, but they have different causes and treatments. Visit our AFib Overview for more insights.
10. How does AFib increase stroke risk?
AFib can cause blood to pool in the atria, leading to clot formation. These clots can travel to the brain and cause a stroke. Blood thinners or left atrial appendage closure procedures like the Watchman device are commonly used to reduce this risk. For more on stroke prevention, explore our AFib & Stroke Risk page.
11. Can AFib be cured?
While AFib is not typically curable, treatments like AFib ablation can help restore normal heart rhythm, reduce symptoms, and improve quality of life. For more information, read our AFib Ablation page.
12. What lifestyle changes can help manage AFib?
Effective lifestyle changes include maintaining a healthy weight, controlling blood pressure, treating sleep apnea, reducing alcohol intake, stopping smoking, and managing stress. These changes can improve AFib outcomes and overall heart health. Learn more on our Lifestyle Impact on AFib page.
13. Is catheter ablation safe, and where should I go for treatment?
AFib ablation is a safe, widely studied procedure and is usually performed in specialized centers. The success rate is high, especially at facilities with extensive experience in AFib ablation. Visit our AFib Ablation page to learn more.
14. Will I need medications after an ablation procedure?
After AFib ablation, many patients experience reduced symptoms and can often discontinue some antiarrhythmic medications. However, those at high risk of stroke may still need anticoagulants. Read more on post-procedure expectations in our Procedure Preparation and Recovery guide.
14. Will I need medications after an ablation procedure?
While treatment can significantly reduce or eliminate symptoms, AFib is typically a chronic condition. Treatments like ablation can improve quality of life and decrease AFib frequency. For more, read Does AFib Go Away?.
16. Can you live a long life with AFib?
Yes, with proper treatment and management, many people with AFib live long, healthy lives. Long-term care may include medications, regular check-ups, and lifestyle adjustments.
17. Can stress trigger AFib?
While stress does not directly cause AFib, it can trigger episodes in people who are predisposed. Stress management is an essential part of a comprehensive AFib treatment plan. Learn about managing stress and other lifestyle factors in our AFib Lifestyle Impact section.
18. Can AFib be triggered by food?
Certain foods, especially alcohol and caffeine in excessive amounts, can trigger AFib episodes. Maintaining a balanced diet and avoiding specific triggers can help manage AFib.
19. Can I drink coffee with AFib?
Moderate caffeine intake has not been shown to increase AFib risk for most people. However, moderation is key, and patients are advised to monitor how caffeine affects them personally. See Caffeine and AFib for more details.
20. Are energy drinks safe if I have AFib?
Energy drinks are not recommended for AFib patients due to high levels of caffeine and other stimulants, which can increase heart rate and potentially trigger AFib episodes. Visit our Energy Drinks and AFib page for more information.
20. Are energy drinks safe if I have AFib?
Sleep apnea, particularly obstructive sleep apnea, is closely linked to AFib. Treating sleep apnea can improve AFib outcomes and reduce episode frequency. Read more on the connection in our Sleep Apnea and AFib section.
22. What is Pulsed Field Ablation, and how is it different?
Pulsed Field Ablation (PFA) is a newer, non-thermal ablation method that selectively targets heart tissue while avoiding damage to surrounding structures. It has shown great promise for its safety and efficiency. Visit our pages about Pulsed Field Ablation and How PFA Compares with Thermal Ablation to learn more.
23. Can sleep apnea affect AFib?
Yes, obstructive sleep apnea is closely linked with AFib. Treating sleep apnea can improve AFib management and reduce the frequency of episodes. Learn more about AFib and Sleep Apnea.
24. What is the Watchman Device for stroke prevention in AFib?
The Watchman Device is a left atrial appendage closure device used to reduce stroke risk in patients with AFib who cannot take blood thinners. Learn more on our page about the Watchman Device.
Section 10: Conclusion and Next Steps
Managing atrial fibrillation (AFib) is a journey that involves understanding the condition, choosing the right treatment options, and making lifestyle adjustments to improve heart health and quality of life. AFib is the most common heart rhythm disorder, affecting millions worldwide, but advancements in treatment options and greater awareness of lifestyle factors have significantly improved patient outcomes.
Key Takeaways:
- AFib Overview: AFib is an irregular heartbeat that increases the risk of stroke and other serious complications. Understanding the different types of AFib, from paroxysmal to permanent, helps tailor the right treatment plan.
- Diagnosis: Early detection of AFib is critical to prevent long-term complications. With wearable devices, monitoring AFib has become more accessible, allowing earlier diagnosis and intervention.
- Treatment Options: Options range from lifestyle changes and medications to advanced procedures such as catheter ablation and the latest Pulsed Field Ablation (PFA). Blood thinners, left atrial appendage closure devices, and lifestyle modifications all contribute to reducing stroke risk and improving outcomes.
- Lifestyle Modifications: Effective AFib management often includes lifestyle adjustments like weight management, exercise, controlling alcohol intake, and addressing sleep apnea, all of which can help reduce the frequency and severity of AFib episodes.
- Long-Term Management: While AFib may not be curable, with the right management strategy, many patients live healthy, fulfilling lives.
Next Steps:
- Consult with an AFib Specialist: Whether newly diagnosed or exploring additional treatment options, consult with a cardiologist or electrophysiologist who specializes in AFib. Dr. Jose Osorio and his team at The AFib Clinic offer personalized care for AFib patients.
- Educate Yourself: Empower yourself with information. This guide and The AFib Clinic website are excellent resources to stay informed on the latest in AFib care.
- Make Lifestyle Adjustments: Implement any necessary lifestyle changes to optimize heart health. Reducing risk factors like weight, sleep apnea, and alcohol use can significantly impact AFib outcomes.
- Stay Committed to Follow-Up: Regular follow-ups help track progress, adjust treatments as needed, and ensure long-term management of AFib.
- Seek Support: Connect with support groups, either in person or online, for those managing AFib. Sharing experiences and learning from others can make a significant difference in coping with the condition.
Remember: AFib is a condition that, while chronic, is manageable. With the right treatment, education, and lifestyle choices, it is possible to lead a long, fulfilling life despite an AFib diagnosis.
For more information or to schedule a consultation, visit The AFib Clinic’s website or call Dr. Osorio’s clinic in Miami, FL, at (855) 444-AFIB.